Thinking about colostrum through a reductionist lens could worsen breastfeeding outcomes
We don't have evidence to suggest that colostral intake alone improves breastfeeding or developmental outcomes
It's important not to think about colostrum's importance through the reductionist lens which is so commonly applied within contemporary health systems.
Although colostrum has hypothetical potential to influence infant immune and metabolic development long-term, there isn’t evidence to demonstrate that colostrum intake alone has clinically relevant developmental impacts in humans.
As Dr Valerie Verhasselt observes in a 2024 review of newborn food intake, there is clear biological plausibility to the theory that colostrum has evolved as "a special fluid to help the newborn transition from intra-uterine and extra-uterine life and lay the foundation for healthy development. [This hypothesis is] supported by the very high levels of microbiota-forming bioactive compounds in colostrum, such as IgA, lactoferrin and human milk oligosaccharides, and high levels of growth and immune factors, including immune cells, all of which are 5–10 times higher than in mature milk and virtually absent in formula. Colostrum may play an important role in guiding immune development in the gut and probably elsewhere, as its period of intake also coincides with high intestinal barrier permeability."
Nevertheless, Dr Verhasselt also confirms that: "the long-term effects of colostrum [itself] on immunity are unknown."
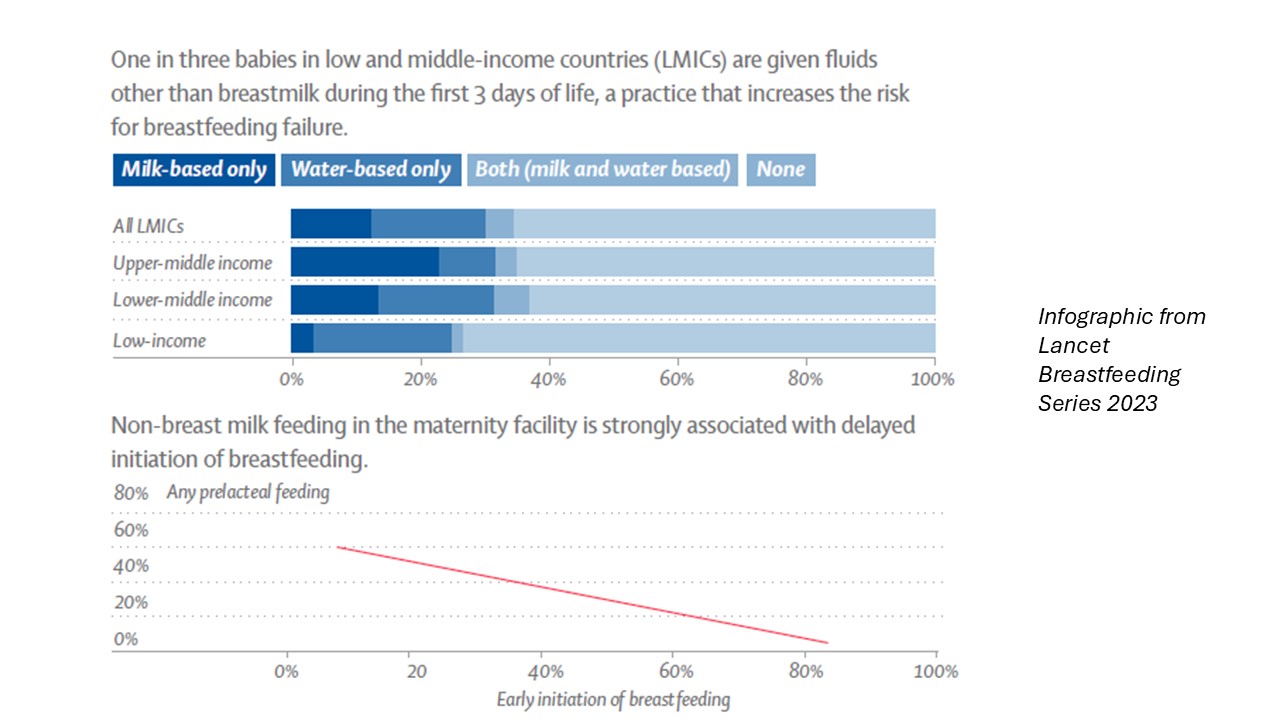
Similarly, the long-term effects of colostrum on infant development are unknown. Some human cultures traditionally discard colostrum. This often occurs, in the 21st century, in low income countries and contexts of socioeconomic disadvantage. The World Health Organisation and other global agencies have instigated programs to re-educate mothers in these societies about the benefits of colostrum, with a view to optimising infant health and immunity in disadvantaged 21st century settings. Prelacteal feeds, which may be used as colstral substitutes, delay initiation of breastfeeding and increase the risk of breastfeeding failure. But there is also no evidence to prove that lack of colostral intake alone resulted resulted, over the centuries of traditional discarding of colostrum in these cultures, in impaired human health and development.
A reductionist approach to colostral intake can worsen breastfeeding outcomes
I propose that it will be difficult to establish long term direct effects of colostrum intake alone because many factors interact in the mother-baby complex adaptive system to shape breastfeeding outcomes and immune and metabolic development from birth onwards, of which colostrum is just one.
I look forward to the day when health systems work to optimise all factors relevant to breastfeeding success, including newborn colostral intake. In this way, we will finally begin to optimise breastfeeding resilience in 21st century mother-baby pairs.
The danger of overemphasising one single factor, such as 'the golden hour postbirth' or colostral intake, is that we might accidentally impact negatively upon multiple other important feedback loops, resulting in unintended outcomes with negative impacts upon breastfeeding success. This could happen through
-
An exaggerated focus on mechanical removal of colostrum which undermines maternal confidence in direct breastfeeding
-
An exaggerated focus on mechanical removal of colostrum which exacerbates maternal anxiety and results in the parental belief that direct breastfeeding (with its small initial volumes) is inadequate to meet an infant's needs
-
An exaggerated focus on use of antenatal colostrum which undermines postbirth milk removal and establishment of supply.
That is, a health system overemphasis on colostrum intake has the potential to worsen breastfeeding outcomes. All elements of clinical breastfeeding support need to be considered in the context of the mother-baby complex adaptive system.
Recommended resources
Skin-to-skin contact after birth is elemental - but the 'golden hour' concept can be unhelpful
Breastfeeding is a symphony of biological (or complex adaptive) systems
The breastfeeding mother-baby pair is a complex adaptive system or CAS (not a dyad)
Selected references
Corona-Cervantes K, S'anchez-Salguero E, Z'arate-Segura P. Maternal immunoglobulins differentially bind a diverse bacterial community in human colostrum and the stool of breastfed neonates. Immunology Letters. 2025;273:106978.
Liben ML. Colostrum: the golden milk for infants' health. Global Journal of Intellectual and Developmental Disabilities. 2017;1(4):GJIDD.MS.ID.555566.
Perez-Escamilla R, Tomori C. Breastfeeding: crucially important, but increasingly challenged in a market-driven world. The Lancet. 2023;401(10375):486-502.
Verhasselt V. A newborn's perspective on immune responses to food. Immunological Reviews. 2024;326:117-129.
